Obesity and Inflammation: Strategies
Last week we discussed how obesity is not just an issue of calories, especially when someone has been obese for a long time. We have a pretty solid picture of obesity setting off a cascade of metabolic syndrome and inflammation. No use just telling someone to eat less when we need to improve their health as a whole.
This sort of approach is why diets like "If It Fit Your Macros" mean well but often send people down a winding path. In the effort to eat "whatever you want" as long as it matches your macros works. I'll admit that. But in my experience it works best when people already have good dietary habits; they eat veggies, whole foods, lean proteins and don't rely on processed health foods or snacks. For everyone else who wants to have their Arctic Zero, Quest Bars, multiple scoops of chocolate cake flavored protein powder, sugar free soda, protein chips and all that other inner fat'kid food, the results aren't always clear cut. I've had quite a few clients trying to force IIFYM with lousy food quality and often times the result is lots of bloating, loose stool, constipation, gas and an over-reliance on things that taste like dessert. If you want to have your cake and eat it too, be prepared to accept the consequences of that cake. And if your cake is loaded with protein powders, sugar alcohols, inulin, highly processed fats and stabilizers, don't be surprised when your digestion is like the back firing car from Uncle Buck.

The point is, I don't believe that just decreasing food intake is all it takes for those with metabolic syndrome and high inflammation. The research, much of what I am referencing from Dr. Pizzorno in the Journal of Integrated Medicine, shows that mitochondrial health requires fewer toxins, more antioxidants, increased muscle mass and optimizing nutrient status......all things that are non-calorie. Don't forget that environment matters too - if you think it doesn't, go to bed tonight with all the lights on. Try to sleep in that environment.
Science-backed stragies to improve mitochondrial health
Fasting
If you remember from last week, I mentioned apoptosis, or "cell death". This is a programmed function that cells use to eliminate poorly functioning or highly stressed cells. Think of it as a cell clean up crew, removing unhealthy cells and organelles to make way for growth and reproduction of healthy ones. But what if the clean crew is impaired? If unhealthy cells are not cleaned up, we end up with uncontrolled cell growth - think cancer, Alzheimer's and atherosclerosis. Overfeeding cells and feeding them a highly inflammatory (think poor food quality) diet stresses them and causes the mitochondria to decrease sensitivity. This is a good place to develop high levels of inflammation, insulin resistance and inability to tap into fat stores. So when we talk about eating less we don't want to start adding in low-quality diet foods (remember the garbage that is Snackwell's? ugh).
Fasting is an effective strategy to decrease mitochondrial stress and allow proper cell death to occur. One key way (besides not ingesting calories of course) is through the activation of AMPK.
AMPK is an enzyme found within your cells. It acts as an energy regulator allowing your cells to do things like
- increase fatty acid oxidation
- stimulate glucose uptake
- stimulate fat utilization and breakdown with muscles
- decrease inflammation
- inhibit cholesterol production
- improve insulin sensitivity
- stimulate new mitochondrial growth
AMPK is there to help you tap into stored nutrients, improve your ability to breakdown fats and carbohydrates, stimulates the cell death and growth of new and healthy cells. Basically all the things we want in a healthy, well-functioning human organisms. One of the reasons drugs like Metformin are tied to decreased cancer risk is because they stimulate AMPK. But fasting does as well. AMPK is activated in a low-energy state, when mitochondria are given a break and no nutrients are coming in for long periods, AMPK is upregulated and we see all the beneficial effects it has like breaking down fat, improving insulin sensitivity and proper cell death. So it's no suprise that over-feeding (obesity) would suppress AMPK and make it consistently harder and harder to lose weight and improve your health.
In essence, fasting is taking your foot off the gas.
Optimizing nutrient status
Like I said before, stop eating low-quality food. I don't mean organic vs non-organic. And I DON"T mean go vegetarian or vegan. I do mean eat your veggies (lots of them) some fruit, lean proteins, high quality fat sources and fibrous carbohydrates. Ditch the fake sugar stuff, the "healthy" junk food, shit that comes in a box or bag. It's great if you can eat organic but I am just trying to get you to put down the protein chips and pick up a carrot.
Low quality foods are more inflammatory. Whether you are aware or not there are always interactions from things like the sweetness of sugar alcohols and insulin, how ingredients will affect your gut microbiome and what kind of oxidative stress highly processed foods are causing the cell. Most processed foods are just void of any sort of vitamin, mineral or antioxidant which are things we need to keep cells running in a healthy manner.
Nutrients that improve mitochondrial function
- CoQ10 - they transport high energy electrons which means fewer free radicals and oxidative damage
- Carnitine - increased ATP production from fatty acid breakdown
- Alpha Lipoic Acid - used with carnitine to clean up excess free radicals from the increase energy production
- Vitamin E - protects mitochondria from oxidative stress
Not to overlook any other nutrients that help improve health of the cell but this shows how just a few make an impact. Don't underestimate the importance of nutrients - I remember reading some research on using whey protein (high in glutathione, an antioxidant) to speed recovery in burn victims.
Reduce exposure to toxins and drugs
Lets start with some basics like not smoking and cutting back on drinking. Both of those are closely tied with mitochindrial stress and damage because of the enormous toll they take on antioxidant status. Other highly inflammatory drugs would be things like acetominophen, NSAIDS, antibiotics, cocaine and statins. All things (along with alcohol and smoking) that are abused by a LOT of people.
Persistent Organic Pollutants(POP) are an issue too. Think pesticides, industrial chemicals and DDT. The World Health Organization even states that Perstent Organic Pollutants can lead to increased cancer risk, reproductive disorders, alteration of the immune system, neurobehavioural impairment, endocrine disruption, genotoxicity and increased birth defects. The Monsanto product, Roundup, was determined this year to have given a groundskeeper cancer (non-hodgkins Lyphoma) and awarded him $289 million. People, this shit is real. If you've been smoking for two decades or abusing NSAIDS then you are stressing the mitochondria in ways they were not meant to deal with.
if you want to see what sorts of health problems are linked to mitochondrial damage, check out this chart below. Hello wrinkles, muscle loss and brain atrophy!
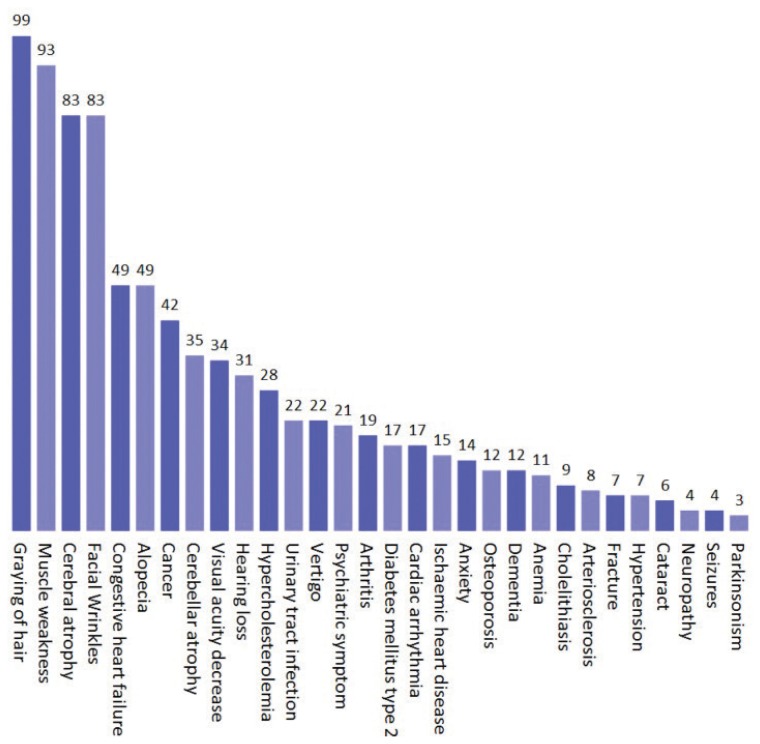
Probability of Mitochondrial Dysfunction in Common Signs, Symptoms, and Diseases
Strength train
After age 25, muscle mass decreases 3-10% per decade if you don't strength train.
Sarcopenia or muscle loss is linked to, among other things, a decrease in Type-2 muscle fibers, loss of motor unites and contractile proteins and.....mitochondrial dysfunction. Things that happen with loss of muscle like decreased ability to produce energy (ATP) and creation of new proteins are improved with maintenance or building of muscle mass.
To make a long story short, building muscle not only helps make you more resilient to ageing process externally (like catching yourself in a fall) but internally too.
Wrapping up
There is a lot of info here but the take-aways are pretty simple. To reduce inflammation, improve mitochondrial health and ALSO lose body fat you need to address more than just calories. But it doesn't have to be super complex. Things like:
- Improve food quality aka stop eating fast food, bagged food, fake health foods and other stuff that isn't whole
- Decrease calorie intake. Yes this does need to happen and it just means eating less but not crash dieting to 1,000 calories per day.
- Implement some fasting. You can try doing a 16/8 fast or just push back breakfast in the morning or choose one day per week to fast for a longer period. Eat more whole complete meals and then don't snack on lots of little stuff in between
- Strength train/build muscle aka lift weights and also get out and walk
- Improve your environment. Make sure sleep quality is high get sun exposure and don't stay up until midnight watching Youtube videos of cats
- Improve nutrient status. Look, everyone wants to say we don't need a Multivitamin but NO ONE is eating all the vitamins and minerals they need. A high quality multi, Vitamin D and minerals will do you a world of good
- Don't smoke, don't abuse drugs or alcohol and prescription meds like antibiotics. Discuss with your doc of course, this is not my area to give specific advice
Decreasing calories is not that hard, people do it all the time through various means: giving themselves half portions, not eating past 6PM, skipping breakfast or what have you. But what about your environment, your food quality, your sleep, your nutrient status? Breaking the cycle of dropping 20-50lbs only to gain it all back, lose muscle in the process and make each subsequent crash diet harder means paying attention to more than just eating less. We need to consider being obese and highly inflamed as not just carrying more bodyfat but a disease state that requires further intervention.
I hope this 2 part series shed light on obesity and moving beyond judging people just because they are overweight as "being a couch potato" or "just eating too much". Perhaps some assumptions about their diets or lifestyles are true to an observer but that doesn't mean judgement is a solution. I am excited to see where the world of obesity research and intervention goes next, I suspect we'll find there is much more behind the curtain that just how much you eat.
References:
Nunnari, Jodi, and Anu Suomalainen. “Mitochondria: In Sickness and in Health.” Cell, vol. 148, no. 6, Mar. 2012, pp. 1145–59. www.cell.com, doi:10.1016/j.cell.2012.02.035.
Pizzorno, Joseph. “Mitochondria—Fundamental to Life and Health.” Integrative Medicine: A Clinician’s Journal, vol. 13, no. 2, Apr. 2014, pp. 8–15.
“Mitochondrial Dysfunction in Obesity.” Life Sciences, vol. 192, Jan. 2018, pp. 26–32. www.sciencedirect.com, doi:10.1016/j.lfs.2017.11.019.
Furukawa, Shigetada, et al. “Increased Oxidative Stress in Obesity and Its Impact on Metabolic Syndrome.” Journal of Clinical Investigation, vol. 114, no. 12, Dec. 2004, pp. 1752–61. PubMed Central, doi:10.1172/JCI200421625.
Brehm, Bonnie J., and David A. D’Alessio. “Environmental Factors Influencing Obesity.” Endotext, edited by Leslie J. De Groot et al., MDText.com, Inc., 2000. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK278977/.
Fung, Dr Jason. “Fasting, Longevity and the Mitochondrial Connection.” Medium, 25 Jan. 2018, https://medium.com/personal-growth/fasting-longevity-and-the-mitochondrial-connection-2aeb857a76a4.
